Using cannabis can have a big impact on your physical and mental health—for better, and once in a while, for worse. That’s why it’s important to consult a healthcare provider before experimenting.
Here at GreenState, cannabis clinician Dr. Leigh Vinocur is here to answer your questions on healthy living with cannabis.
Editor’s Note: The answer to this question is meant to supplement, not replace, advice, diagnoses, and treatment from a healthcare provider. Always consult a medical professional when using cannabis for medicinal purposes, and do not disregard the advice of your healthcare provider because of anything you may read in this article.
Q: Can I use cannabis with my immunotherapy cancer treatment?
I get asked this question a lot. We know that the endocannabinoid system has many CB2 receptors in our immune system, and it plays a big role in modulating and maintaining the balance of our immune system. Therefore, cannabis which interacts with those receptors, also affects our immune system.
In fact, cannabis has been found to dampen the immune response. Thus, it has been used to decrease inflammation and the inflammatory response seen in many chronic diseases, such as arthritis. Additionally, cannabis may act as neuroprotective, and it may dampen neuroinflammation. That is why it is often used during chemotherapy to mitigate the chances of nerve damage from chemotherapy-induced peripheral neuropathy (CIPN).
What are immunotherapies?
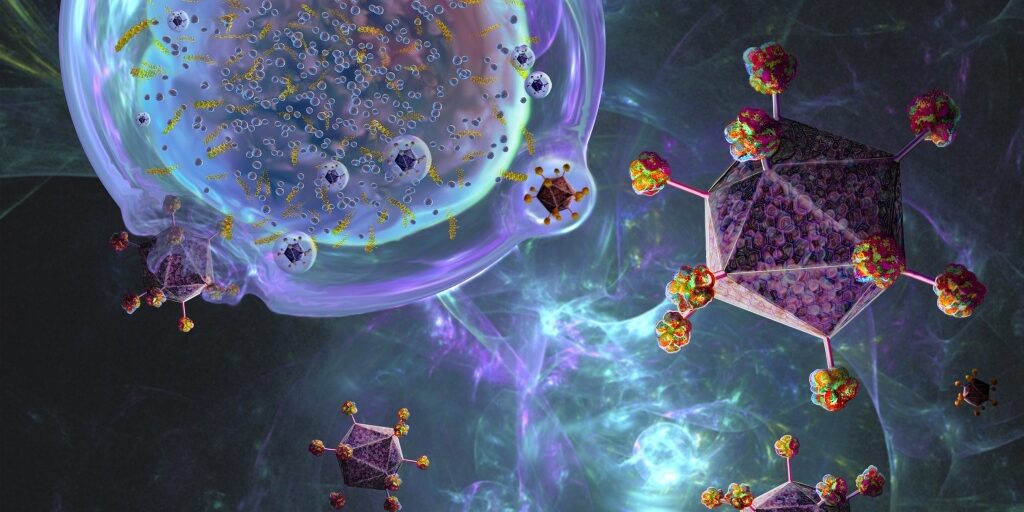
Immunotherapy is a more recent and innovative type of cancer treatment called targeted therapy, designed to go after genetic mutations within specific cancers. These therapies are developed to use our immune system to fight cancer. Several commonly used therapies are cancer vaccines, and monoclonal antibodies called immune checkpoint inhibitors (ICI). The big question here is, how does cannabinoid therapy affect these types of cancer treatments?
Cancer vaccines used for therapy work similarly to vaccines meant to prevent certain diseases. They expose our body to specific proteins expressed by cancer cells and induce our immune system to fight cancer that way. Two common examples are Talimogene laherparepvec (T-VEC) for advanced melanoma, and Sipuleucel-T (Provenge), used for advanced hormone-resistant prostate cancer.
Immune checkpoint inhibitors (ICI) are monoclonal antibody-targeted therapies. They boost our immune system by stopping immune checkpoints. A specific immune white blood cell called T -cells express checkpoint proteins that turn on and off our immune response to protect our healthy normal cells while killing invading organisms and abnormal cells.
Many cancers have developed ways to make these checkpoint proteins turn off our immune response, allowing them to grow unchecked and disguised to our T-cells. These checkpoint inhibitor therapies block these proteins and turn our immune system back on so our T-cells can find, fight and kill the cancer cells.
Most of these medications’ names end with “ab” since they are monoclonal antibodies. However, very common drugs that many people have heard of through TV commercials marketing to cancer patients for various types of cancer are PD-1 inhibitors. The most common PD-1 inhibitors are Nivolumab (Opdivo) and Pembrolizumab (Keytruda).
Does the research show that you can use cannabis with these immunotherapies?
Unfortunately, right now, the research has been mixed. Because we know cannabis can dampen our immune response and the immunotherapies described above are intended to rev up our immune system to kill cancer, there are legitimate concerns.
A study from Israel in 2019 looked at Nivolumab (Opdivo) and cannabis use together. It found that the response rate of the treatment was reduced when combined with cannabis. However, there was no statistical difference in the progression-free survival or overall survival.
This means that even if the cannabis and the Nivolumab group’s immune response were not as robust as the Nivolumab group alone, both had the same amount of time disease-free, and their overall survival times were the same.
However, a study published in 2020 by the same researchers found cannabis consumption with immunotherapy was found to cause a decrease in both tumor progression times. This meant the tumor spread more quickly, with overall survival reduction, cautioning its use. Although, it did seem to protect against many of the side effects seen with immunotherapy.
The limitations of the research were that both studies were relatively small populations of patients, and the researchers speculated that often the patients seeking cannabis had worse health and prognosis in the first place.
A more recent study published in February 2023 by many of the same researchers in Israel looked at the correlation between cannabis and clinical outcomes in patients with metastatic non-small-cell lung cancer (NSCLC) taking Pembrolizumab (Keytruda). They found that cannabis use did not shorten the time to cancer progressing, and it was not an independent predictor of mortality. They also published data using a mouse model and found that it did not decrease the efficacy of a PD-1 inhibitor.
Nevertheless, as a cannabis physician, I currently recommend extreme caution when patients inquire about cannabis use during immunotherapy, and I often dissuade them from using it during their therapy. We need much more research to definitively assess the risks and benefits of cannabinoid therapy in conjunction with targeted immunotherapy.
Therefore, to answer the initial question above: at the present time, I warn against medical cannabis therapy during immunotherapy for cancer.
Got cannabis questions? Ask Doctor Leigh. Send your questions to GreenState’s Editor at [email protected] and keep an eye out for new answers from Dr. Leigh Vinocur every month.
Dr. Leigh Vinocur is a board-certified emergency physician who also has a cannabis consulting practice for patients and industry. She is a member of the Society of Cannabis Clinicians and a graduate of the inaugural class, with the first Master of Science in the country in Medical Cannabis Science and Therapeutics from the University of Maryland School of Pharmacy.
The response to this question was not written or edited by Hearst. The authors are solely responsible for the content.
Originally published on Greenstate.com, June 5, 2023.