The liver is our major detoxifying organ. It plays an important protective role in drug metabolism in oral preparations that go through first-pass metabolism[1]. A group of enzymes in the liver is part of the cytochrome P450 system. It allows us to metabolize drugs we ingest orally. Often the liver metabolizes drugs into inactive compounds that can be eliminated by our bodies.
However sometimes our livers create active metabolites that can have either an equal or greater effect than the original parent compound/drug. And these metabolites may be responsible for the actual therapeutic effects or they can augment the therapeutic effect[2] of the drugs.
Additionally, there is a subset of active metabolites coming from compounds/drugs called prodrugs[3] [4]. Prodrugs are medications or compounds that are completely inactive until metabolized to their active compound in the body. For example, codeine[5] [6] is a prodrug that does not have analgesic properties until the enzymes in the cytochrome P450 system, specifically CYP2D6 mediated oxidation, turns it into the active metabolite of morphine.
Often these prodrugs are created intentionally by drug manufacturers as a way to get a compound into the body by improving bioavailability, especially if the original compound isn’t well absorbed through the GI tract.
Some active metabolites can have the same or even slightly different effects as the parent drug. An example of this is the tricyclic antidepressant imipramine[7], which blocks the uptake of both serotonin and norepinephrine in the brain. This drug’s active metabolite is an N- desmethylated derivative called desipramine. It only blocks the uptake for norepinephrine. It does not do the same for serotonin. Individual factors[8] that affect first pass metabolisms such as age, concomitant food, medication ingestion, and genetics related to enzyme activity, may account for why some patients have different and varying degrees of responses and side effects to this medication and other medications undergoing first-pass.
Understanding and studying the pharmacokinetics and pharmacodynamics of drugs and their metabolites is critical with important clinical indications. There are potential drug-drug interactions with drugs, prodrugs, and/or their active metabolites that can cause toxic effects when different drugs compete for the enzymes in the Cytochrome P450 system.
An example of this was seen with terfenadine[9], a drug marketed as the first non-drowsy antihistamine under the brand name Seldane. By accident, it was found to be a dangerous prodrug for an active metabolite called fexofenadine, after it was converted to its acidic form by the CYP3A4-catalyzed oxidation of its methyl group to a carboxylic acid. This active metabolite also worked as an antihistamine and it turned out to be much safer. In its native parent compound form of terfenadine, if not metabolized quickly and it accumulated in the body, it was found to cause the fatal tachyarrhythmia due to QT prolongation called torsade des points. This was seen more often when there was concomitant administration of some antibiotics (often prescribed with antihistamines) that interfered with or inhibited the CYP3A4-catalyzed oxidation. Therefore, it was withdrawn from the market due to the resulting deaths. However, the acid form of fexofenadine then went on to be marketed and become the popular non-drowsy antihistamine, Allegra.
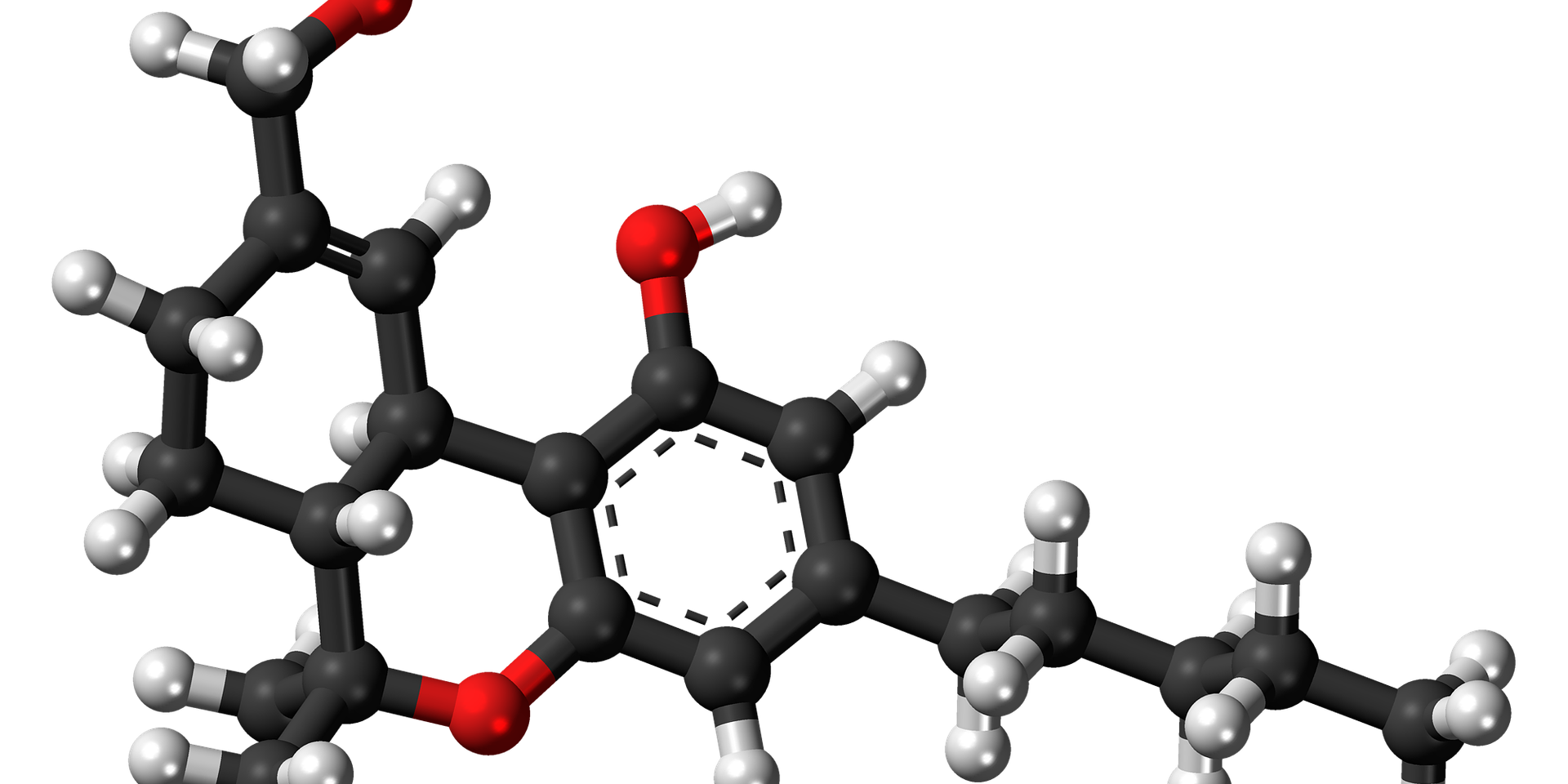
THC is a cannabinoid that also has an active metabolite. When delta-9-THC is ingested orally like other medications due to first-pass metabolism it has a relatively low bioavailability, between 10-20%[10]. However, during first-pass THC is metabolized by the cytochrome P450 system enzymes CYP2C9[11] [12] [13] to its active metabolite 11-hydrox-THC in a one to one ratio. This metabolite is three to seven times more potent than THC and more readily crosses the blood-brain barrier [14] [15] [16].
The clinical implications of oral ingestion of THC with its very potent active metabolite could lead to an accidental overdose. Due to the longer and delayed onset of action that can be up to 1-2 hours,[17] sometimes people take repeated doses of their infused gummies thinking the initial dose is not working. And while an overdose is not fatal the way opioids are, the symptoms of acute cannabis intoxication can be very uncomfortable, especially for naïve users. They include nausea, vomiting, tachycardia, hypertension, confusion, obtundation, ataxia, anxiety, paranoia, loss of reality, and rarely seizures have been reported[18]. Not to mention the risk of these infused candies or other sugary THC treats, getting into the hands of toddlers and children.
Just like any other medication, but maybe even more so with tempting candy preparations of cannabis, they must be kept in a safe place away from children. Many states allowing edibles are now creating legislation to have maximal doses per serving with childproof containers. And adults need to be cognizant of the delayed onset of action as well so that they do not take repeated doses or servings until they have allowed for the time to start to feel the effects of the medication.
[1] Pond S., Tozer T., First Pass Metabolism Basic Concepts and Clinical Consequences. Clin Pharmacokinet. 1984; 9(1): 1-25.
[2] Garattini S., Active Drug Metabolites: An Overview of their Relevance in Clinical Pharmacokinetics. Clin Pharmacokinet. 1985; 10: 216-227.
[3] Ortiz de Montello, P. CytoChrome P450-activated Prodrugs. Fut Med Chem. 2013; 5(2): 213-228.
[4] Waller D., George C., Prodrugs. Br J Clin Pharmaco. 1989; 28: 497-507.
[5] Horn J., Hansten J., Narcotic Anaglesics Metabolized by CYP2D6. Pharmacy Times. Published May 1, 2005. https://www.pharmacytimes.com/publications/issue/2005/2005-05/2005-05-9511. Accessed Novmember 20, 2019.
[6] Smith H., Opioid Metabolism. Mayo Clin Proc. 2009; 84(7): 613-624.
[7] Garattini S., Active Drug Metabolites: An Overview of their Relevance in Clinical Pharmacokinetics. Clin Pharmacokinet. 1985; 10: 216-227.
[8] Pond S., Tozer T., First Pass Metabolism Basic Concepts and Clinical Consequences. Clin Pharmacokinet. 1984; 9(1): 1-25.
[9] Renwick A., The Metabolism of Antihistamine and Drug Interactions; The Role of Cytochrome P540 Enzymes. Clin Exper Allergy. 1999; 29(3): 116-124.
[10] Huestis M., Human Cannabinoid Pharmacokinetics. Chem Biodivers. 2007; 4(8): 1770-1804.
[11] Watanabe K., Yamaori S., Funahashi T., Kimura T., Yamamoto I., Cytochrome P450 enzymes Involved in the Metabolism of Tetrahydrocannabinols and Cannabinol by Human Hepatic Microsomes. Life sciences. 2007; 80: 1415-1419
[12] Mc Gilveray I., Pharmacokinetics of Cannabinnoids. Pain Res Manage. 2005; 10(Suppl A): 15A-22A.
[13] Schwilke E., Heustis M., et. al. Delta-9-tetrahydrocannabinol, 11-Hydroxy-THC and 11-Nor-9-carboxy-THC Plasma Pharmacokinetics during and after Continuous High-dose oral THC. Clin Chem. 2009; 55(12): 2180-2189.
[14] Grotenhermen F. Pharmacokinetics and Pharmacodynamics of Cannabinoids. Clin Pharmacokinet. 2003; 42(4): 327-360
[15] Lemberger L., Rowe H., et. al. Comparative Pharmacology of Delta-9 Tetrahydrocannabinol and its Metabolite 11-Hydroxy Tetrahydrocannabinol. J Clin Invest. 1973; 52(10): 2411-2417
[16] Goncalves J., Duarte A., et. al. Cannabis and Its Secondary Metabolites: Their Use as Therapeutic Drugs, Toxicologic Aspects and Analytic Determination. Medicnes( Basel) Online. Published February 23, 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6473697/. Accessed November 21, 2019.
[17] Vandrey R., Cone E., et. al. Pharmacokinetic Profile of Oral Cannabis in Humans: Blood and Oral Fluid Disposition in Relation to Pharmacodynamic Outcomes. J Anal Toxicol. 2017; 41(2): 83–99.
[18] Wang, S., Cannabis: Acute Intoxication. Uptodate.com. Updated October 22, 2019. https://www.uptodate.com/contents/cannabis-marijuana-acute-intoxication. Accessed November 21, 2019.